
Check Out Our New Forum!
The Your Turn Forum provides a space where people can post questions about mesh and medical device related issues and get advice and support from the Mesh News Desk community.
Join the Discussion!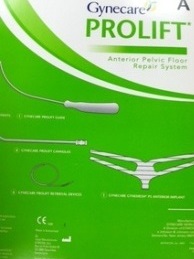
She sits in a downtown Atlanta apartment. “Mandy” is 71 years old. She was implanted with a Prolift, made by Ethicon, a division of Johnson & Johnson, a decade ago. Mandy (who is involved in litigation and can’t use her real name) tells MND she rarely leaves her home. She is in constant pain which is treated with her constant companion, morphine. At least it keeps the pain bearable and allows her some interaction with her family.
The date would come too late for Mandy and thousands of others implanted with transvaginal mesh to treat pelvic organ prolapse (POP).
The date was January 5, 2016.

The U.S. Food and Drug Administration announced mesh for POP would be officially reclassified as class III, reserved for high-risk devices or questionable devices that nonetheless might be needed to sustain life.
POP mesh, a larger plastic mesh made of polypropylene (PP) and implanted through slices in the vagina (transvaginally), had proven to deliver at least as much harm as good. Complications were “not rare,” the FDA concluded in 2011, an about-face from three years earlier when the agency called transvaginal mesh complications “rare.”
“It is not clear that transvaginal POP repair with mesh is more effective than tradition non-mesh repair,” said the FDA on July 13, 2011.
In regulatory language, the FDA said “the risk-benefit profile of surgical mesh for transvaginal POP repair is not well established.”

Industry reaction was swift.
Even though the announcement gave mesh makers 30 months to act, POP mesh makers - Ethicon (Johnson & Johnson), Boston Scientific, American Medical Systems, and C.R. Bard, quickly and quietly moved to voluntarily recall their POP meshes from the market.
In doing so, they could evade the imposed vigorous premarket approval (PMA) process reserved for drugs, and class III devices, costing manufacturers millions in research and clinical trials.
July 2018 marks the end of 30 months! Polypropylene mesh used to treat POP is now officially classified as High-Risk, its use restricted for transvaginal implantation unless industry can prove through years of costly clinical trials its mesh is safe and effective.
Doctors or hospitals can no longer exhaust the supply they might have had on their shelves, though an FDA spokesman says the agency does not have the authority to check doctor’s use of the mesh.
Polypropylene mesh used for stress urinary incontinence, also known as a “sling,” or a “ribbon,” or “hammock,” is not only still on the market but is heralded as the Gold Standard by one medical society, AUGS.

Pelvic organ prolapse meshes are generally larger than mesh used to treat incontinence, and have arms that anchor them into deep tissues, muscles and ligaments. Mesh removal experts consider them particularly difficult to remove.
Tens of thousands of product liability lawsuits since 2012 may have already delivered a death knell. One by one, POP mesh has disappeared from the market.
Pinnacle Pelvic Floor Repair, a POP mesh kit made by Boston Scientific was taken off the market May 10, 2011 in an “URGENT MEDICAL DEVICE RECALL – IMMEDIATE ACTION REQUIRED.” The device “may exhibit low tensile strength between the needle and suture and led to needle detachment during mesh leg placement,” said the company.
Prolift and Prolift +M were quietly removed by Ethicon (J&J) in June 2012, as was Prosima Pelvic Floor Repair System. C.R. Bard took its Avaulta mesh off the market in 2012.
Elevate and Apogee, made by American Medical Systems, went away when the company was sold to Endo, which later closed its women’s health division.
Restorelle by Coloplast is still used for POP repair.
AUGS, the American Urogynecologic Society, convened a POP Mesh Consensus Conference in 2016 to promote its patient advocates who promote the continued used of mesh as a treatment for pelvic organ prolapse. POP mesh proponent, Sheri Palm of APOPS is among them.
But as of today, POP mesh is essentially gone, unless it is used overseas or implanted through the abdomen.
The FDA cannot reveal if there are any pending applications for POP mesh. It’s held under wraps as a trade secret and/or confidential commercial information, but you can check the PMA new application field in the FDA website, after the mesh is approved.


In other words, the post-approval monitoring of POP mesh may serve the now FDA requirement of a higher bar for proof and safety, the PMA.
MND has made a request to other mesh makers. We are still waiting a reply.
Yet, researchers are optimistic.
Multiple “White Papers” conducted by researchers (for profit) predict the pelvic implant market will reach $300 million in a decade with use rising in China and third world countries.

There is a loophole for manufacturers to continue to use POP mesh and it doesn't require a PMA. Any device implanted abdominally can still be used for such application exclusively.
The FDA reclassification only covers transvaginal implantation. Abdominal application remains class II, moderate risk.
An FDA spokeswoman says the agency does not have regulatory power to check doctor’s offices, nor would it do so.
“Mesh placed abdominally for POP repair appears to result in lower rate of mesh complications compared to transvaginal POP surgery with mesh,” the FDA concluded in a 2011 patient safety warning. Some surgeons agreed abdominal sacral colpopexy (ASC)”is an excellent procedure for treating POP,” according to a surgeons working group in response to the suggestion to reclassify.
So abdominal placement and using the 522 studies in place of a PMA or to supplement it, could be the loophole opening to reintroduce POP mesh on the market.

As part of the Federal Food, Drug and Cosmetic Act, established in May 1976, three categories of devices were established, with class I as the lowest risk devices such as a wheelchair or Band-Aid, class II such as a defibrillator, and class III for higher risk devices requiring pre-market approval.
One might surmise that a permanent implant should automatically fall into a high-risk category, but that didn’t happen.
When transvaginal mesh hit the market in the late 1990s and early 2000's, it was classified as class II and entered the market with an exchange of paperwork under the 510(k) approval process – approved for marketing – no clinical trials required.
All an applicant had to do was name another marketed mesh - the “substantial equivalent” - as a “predicate” as part of the paper exchange.
It didn’t matter if that predicate had been removed from market for being defective.
ProteGen served as a predicate device for about 60 different pelvic meshes, according to researcher Suzanne McClain. But ProteGen, one of the first pelvic meshes on the market in 1996, was taken off three years later. It does “not appear to function as intended” and led to a higher rate than expected of vaginal erosion and wound rupture at a surgical incision. Never mind.
Mentor, Ethicon, American Medical Systems, Gyne Ideas, Tyco, Caldera all either named ProteGen as their direct or indirect predicate (substantial equivalent). But there is no mechanism within the FDA to trigger a review of devices that named ProteGen as its predicate, even though there is an FDA presumption and reasonable assurance of safety and effectiveness for the predicate device.

Industry knew this and liked the 510(k). A 510(k) application might create a wait time of 90 days and cost a few thousand dollars. With that easy- breezy opening, mesh makers, mindful of competition, entered the market in droves.
A report in the BMJ on POP meshes found 61 devices whose approval relied on claimed equivalence to Mersilene Mesh and ProteGen. There were no clinical trials evidence for those 61 devices at the time of approval.
After receiving nearly 4,000 reports of mesh-related complications, including deaths, in September 2011, the FDA convened its first expert panel on transvaginally-placed polypropylene mesh implant. It left with the conclusions that incontinence mesh should stay on the market but POP mesh raised some troubling questions and should be reclassified.
No action was taken by the agency until January 2012.
After receiving even more reports of mesh-related complications, including organ perforation and bleeding, vaginal mesh exposure, pelvic pain, mesh shrinkage, painful sex and infection, the FDA issued orders for post-market surveillance studies to 33 manufacturers of urogynecologic surgical mesh for POP. Seven manufacturers of incontinence slings were also ordered to undergo three-years of post-approval monitoring of pain, infection, painful sex, vaginal scarring and shrinkage, vaginal bleeding and discharge, fistula formation, and the quality of life, among implanted patients.
The FDA recommended randomized clinical trials or prospective cohort study design. Over the next three years, industry would be required to submit quantifiable assurances to the FDA that their POP implant were safe and effective, now requiring some heavy lifting. Instead, POP meshes quietly disappeared.
The FDA today says that in most cases, POP can be treated successfully without mesh, “thus avoiding the risk of mesh-related complications.”
According to the agency doctors should warn their patients that:
“Removal of mesh due to mesh complications may involve multiple surgeries and significantly impair the patient’s quality of life. Complete removal of mesh may not be possible and may not result in complete resolution of complications, including pain.”
Why not a complete ban? In 2011, the FDA concluded there was insufficient evidence to support the ban or recall of POP mesh, even as one mesh opponent, a Ms. K. commented to the Federal Register:
Dr. Antonio Pizarro submitted:
“Until we can prove that the benefits of mesh repair over non-mesh repair outweigh its significant risks, we should abandon the use of these problematic materials in the care of women with prolapse. There exists a danger that if the FDA does not ban mesh, surgeons will continue to rationalize the available data and obfuscate the plain reality facing us as surgeons—that mesh provides no proven advantage to women suffering from prolapse over repairs not using mesh. This obfuscation will lead to the continued use of mesh if we allow it to do so.”
Surgeons signing onto a working group on POP mesh advanced, “We are deeply concerned that the current process could, as an unintended consequence result in a major setback to those core goals for many providers successfully utilizing mesh and observing high rates of satisfaction and superior outcomes.”
With the final reclassification, advocates and opponents may not be satisfied, but the reclassification creates one more hurdle for industry to scale. Proving safety of devices with a long, troubling history may be impossible and economically foolish to try.
Mesh for stress urinary incontinence (SUI) remains on the market, in a class II status with seamless entry into the market even though the majority of defective product cases currently filed involve SUI polypropylene mesh.
The reclassification comes too late for Mandy, Carleen, Linda, and countless other women who live with a permanent polypropylene POP mesh and whose lives are forever changed. ###
MND, January 4, 2016, FDA Rules to Reclassify POP Vaginal Mesh as High Risk! (here)
Federal Register, January 5, 2016, Obstetrical and Gynecological Devices; Reclassification of Surgical Instrumentation for Use with Urogynecologic Surgical Mesh (here)
FDA Urogynecologic Surgical Mesh: Update on the Safety and Effectiveness of Transvaginal Placement for Pelvic Organ Prolapse,
July 2011 (here)
FDA, Concerns about Surgical Mesh for POP, July 13, 2011 (here)
MND, Jan. 2012, Mesh Makers who Received 522 PostMarket Surveillance Orders (here)
MND, March 2013, SUI Injury Reports to FDA up 36 Percent (here)
FDA Final Order - Letter to mesh makers for 522 studies, January 2012 (here)
MND, January 9, 2012, Mesh Makers who Received FDA Letter Requiring Postmarket Surveillance (here)
MND, AUGS Prolapse Consensus Conference Announced with Patient Advocates, October 16, 2016 (here)
Time to rethink: an evidence-based response from pelvic surgeons to the FDA Safety Communication:
“UPDATE on Serious Complications Associated with Transvaginal Placement of Surgical Mesh for Pelvic Organ Prolapse”
from the Pelvic Surgeons Network, January 2012 (here)
MND, What Happened to the FDA Request for Transvaginal Mesh Studies? September 19, 2012 (here)
June 4, 2012, Ethicon letter to Judge Goodwin, it plans to stop commercialization of four meshes (here)
MND Mesh-Injured Patient Researches ProteGen Mesh Predicate, November 8, 2011 (here)
News Release, April 4, 2018, Female Pelvic Implants Market to reach a value of over US $300 Mn by the End of 2027 (here)
BMJ, December 2017, Trials of transvaginal mesh devices for pelvic organ prolapse: a systematic database review
of the US FDA approval process (here)